Bariatric surgery, known widely as a weight loss surgery, is a surgical operation done on people with obesity to shed weight. It is mainly recommended when other weight loss methods fail and the patient’s health is at risk.
The surgery procedure work in a way that it modifies the digestive system mainly the stomach and at times the small intestine. It regulates how many calories you can consume and absorb. In other instances, it also reduces hunger pangs signals traveling from the digestive system to the brain.
Additionally, the procedures help treat and prevent other metabolic diseases such as fatty liver disease, and diabetes related to obesity. However, the same procedure comes with side effects like hair loss because of the drastic dietary and metabolic changes leading to nutritional deficiencies.
Therefore, understanding the procedure and how to manage it later will help you navigate the post-surgery phase with confidence.

Reasons for Bariatric Surgery
Bariatric surgery is one of the most successful treatments for class III obesity. Studies from National Institutes of Health (NIH), shows it’s nearly impossible for class III obesity people to manage weight loss through exercise and dieting alone. Once the body recognizes the higher weight as normal, it strives to return to that weight despite the method you use for weight loss. Understanding this phenomenon, weight loss bariatric surgery changes how the body manages your consumption, giving room to healthy dieting and overall lifestyle changes to sustain the weight loss and health.
Conditions Bariatric Surgery Treatments
Obesity is often associated with chronic illnesses that may be life-threatening. After surgery, many report the conditions and associated risk factors do improve because of the weight loss. The conditions you may be at risk of include:
- High blood pressure: also known as hypertension implies the force of blood flowing through blood vessels is high. The high force wears down walls of the blood vessels putting you at risk of stroke or heart attack.
- High cholesterol: Also referred to as hyperlipidemia means your blood has many fats which could add up and block your blood vessels. This why high cholesterol levels in your body puts you at risk to stroke or heart attack.
- Type 2 diabetes: Excess fat in your body may lead to insulin resistance resulting to type 2 diabetes. The risk of contracting type 2 diabetes does increase by 20% for every 1-point increase on body mass index scale.
- High blood sugar: Hyperglycemia is linked to insulin resistance and a considered precursor to diabetes. If not treated, it can damage your blood vessels, nerves, tissues and organs increasing risks to other diseases.
- Heart disease: Obesity leads to congestive heart failure and impaired cardiac function. It causes a plague to buildup in the arteries increasing risks of stroke and heart attack.
- Kidney disease: The metabolic syndromes linked with obesity such as, insulin resistance, high blood pressure and heart failure are the greatest contributors to kidney failure and chronic kidney disease.
- Osteoarthritis: When you have excess weight, the pressure is exerted on joints like your knees. This makes it possible to develop osteoarthritis or worsen it if you already have it.
- Obstructive sleep apnea: People having sleep apnea have difficulty in breathing in their sleep when their respiratory tract gets blocked. This reduces oxygen flow to important organs like the heart endangering their lives.
- Cancer: Obesity is correlated with risk of contracting more types of cancer though the connection isn’t well understood. It also increases death from cancer by 50%.
Types of Bariatric Surgery
There are different types of weight loss bariatric surgery conducted to manage obesity. They include:
Gastric Sleeve
The gastric sleeve or sleeve gastrectomy is the most commonly performed bariatric surgery. This is because it’s a simple and safe procedure with little risk of complications on most people. The procedure removes a huge portion of the stomach, about 80% leaving a small, tubular portion which resembles a sleeve. This reduces the portion of food you can take in a sitting making you full faster. This stabilizes your metabolism by decreasing appetite and regulating blood sugar.
Gastric bypass
Also referred to as “Roux-en-Y,” is a procedure where the small intestine ends up in the Y form. In this weight loss surgery, the surgeon creates a small pouch on top of the stomach, splitting it from the lower section using surgical staples.
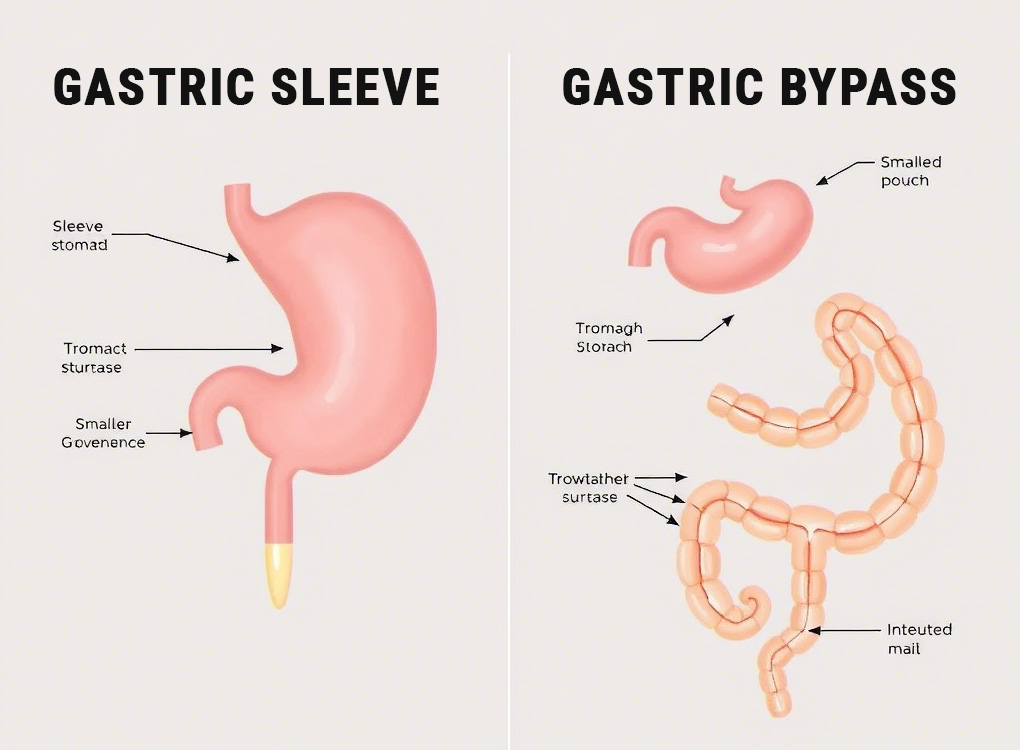
Then they divide the small intestine and bring the new segment connecting it to the stomach pouch. This way, food now flows via the smaller stomach and lower segment of the small intestine and not any other. This restricts the amount of food your stomach can hold and how much nutrition the intestine can absorb.
Biliopancreatic Diversion with Duodenal Switch (BPD-DS)
This is the duodenal switch, a procedure combining sleeve gastrectomy and intestinal bypass. Though its similar to Roux-en-Y, the procedure is more extreme as it bypasses the small intestine by about 75%.
It reduces hunger hormones produced in the small intestine and the stomach by restricting the amount of nutrition the small intestine absorbs. Though it’s an effective surgery for weight loss, it can make it hard for the body to absorb enough nutrients to stay healthy.
Stomach Intestinal Pylorus Sparing Surgery (SIPS)
The SIPS is a newer procedure where the original duodenal switch is modified to eliminate complications. It’s also referred to as Loop Duodenal Switch or SADI-s. Studies are still in early stages but it’s promising to replace duodenal switch.
It also starts with a sleeve gastrectomy that divides the small intestine after the stomach. Though here, the small intestine gets attached as a loop that only requires one surgical connection instead of two. This means less of the small intestine gets bypassed to allow for more nutrients absorption.
Risks and Benefits of Bariatric Surgery
When thinking about the pros and cons of bariatric surgery, it’s vital to factor in the risks of the procedure and possible side effects after the operation.
Surgical Complications
All surgical procedures have a certain level of risk. The longer and complex a procedure is; the more risk it has. Here are the surgical complications that may arise:
Pros of Bariatric Surgery
There are a number of benefits of bariatric surgical procedures. They include:
- Significant and sustained weight loss: Bariatric surgery is the only treatment approved as effective in managing class III obesity.
- Improved metabolism and reduced hunger hormones: The surgery is the only treatment rewiring the body’s metabolic programming after a person is obese to prevent future weight gain.
- Blood sugar and cholesterol management: Weight loss surgery remits diabetes symptoms and allows people having varied metabolic syndromes to stop the medications.
- Guarantees a longer and healthier life: Having a bonus of reducing diseases and other discomforts associated with obesity, the surgery can extend a life. Scientific studies reveal that bariatric surgery reduces risks of death by over 40% from any cause.
Cons of Bariatric Surgery
Surgeries to correct the digestive system may cause specific digestive complications. Sometimes, they are referred to as post-gastrectomy syndromes and include:
- Malabsorption and malnutrition: A number of bariatric surgery procedures induce malabsorption in the small intestine to reduce calories absorption. Malabsorption may lead to loose stools and nutritional deficiencies if you don’t take keen consideration. To prevent this, your health provider should prescribe nutritional supplements to act as a boost.
- Dumping syndrome: This refers to multiple symptoms that occur when the stomach dumps food fast in the small intestine. Statistics show that up to 50% people with bariatric surgery often have dumping syndrome symptoms after sometime. They can include diarrhea, nausea, abdominal cramping, and hypoglycemia. Though the symptoms fade with time, your healthcare provider should provide clear dietary guidelines to prevent or reduce the syndrome till full recovery is realized.
- Gallstones: Rapid loss of weight sends a huge chunk of cholesterol to the liver for processing. When the liver in turn sends bile to the gallbladder, it also carries extra cholesterol. The cholesterol can build up in the gallbladder causing cholesterol gallstones. Though gallstones don’t amount to any problem. However, they may travel and get stuck in the bile ducts causing a health risk. Your doctor may prescribe for you some medicine to prevent gallstones after a surgical operation.
- Bile reflux: A surgical operation affecting the pyloric valve (opening between the stomach and small intestine) can cause a malfunction. In case the pyloric valve doesn’t close well, the result is bile reflux. Meaning, the bile sent by your gallbladder to the small intestine to aid in food digestion can backwash into the stomach. The risks of bile reflux are eroding the stomach lining causing stomach ulcers and gastritis.
Hair Loss After Bariatric Surgery
After bariatric surgery, many patients face hair loss problems which stem from both the fast weight reduction and dietary problems. Patient data shows that 57% of individuals lose hair during the three to six months after their bariatric surgery. The condition is known as telogen effluvium, which develops when the body chooses vital operations instead of maintaining hair growth.
Nutritional deficiencies act as a crucial factor that leads to hair loss after the surgical procedure. Usually, when essential nutrient levels decline, including protein, biotin, zinc, iron, Vitamin B12, and vitamin D, the hair strands move into an early resting phase, resulting in heavy hair loss.
However, this type of hair loss occurs only for a short period. Most patients will experience hair regrowth between six and twelve months after making the appropriate dietary changes and consuming recommended protein levels and supplementary treatments.
Prolonged hair loss after six months requires medical assessment to check any ongoing health issues that need professional attention. Before starting any dietary treatment, seek guidance from a medical provider about the appropriate nutrients for maintaining weight loss goals
Bottomline
Class III obesity is hard to beat and with no proper care, it’s life-threatening to the lives of many people. It can cut short the quality of life of and individual and the lifespan in totality.
The good news is that bariatric surgery offers a long term solution to the difficult and most progressive disease. It can change the biological factors and work against all odds for people with obesity to shed weight.
While a surgery may have its own risks and complications, bariatric has lower risks levels. Engage the doctors to know more to enjoy your journey in better health.
The fact is that nutritional depletion following bariatric surgery can lead to protein wasting, loss of iron, depletion of biotin, B12, Vitamin A, Vitamin D, calcium, zinc, magnesium, fatty acids, and sufficient calories each day. This can lead to stress on the hair shaft. Very few structures metabolize as rapidly as hair. This means that hair needs more nutrition daily than other body structures. When protein is lost in sufficient quantities along with vitamins and minerals, hair shafts cease to elongate, go into the resting phase, and shed. All the factors lead to hair loss. The question is whether this hair loss is permanent. This has not been properly addressed over time, but it needs to be evaluated.
Bariatric (Weight Loss) Surgery: Metabolic, nutritional, psychological and physiological Consequences
You will often see sources that recommend protein, biotin, silica, and snake oil shampoos such as Nioxin to promote hair growth following bariatric surgery. Many of these sources are just trying to sell your products because you have hair loss and it bothers you. They often suggest a single product and offer to sell it to you. Perhaps dietary manipulation will help to retard hair loss, but it may be that you must reverse the bariatric surgery to overcome the associated hair loss from long-term nutritional depletion.
Frequently Asked Questions
What is Bariatric Weight Loss Surgery?
Bariatric weight loss surgery refers to a range of surgical procedures designed to help individuals who are severely overweight or obese lose weight. These surgeries work by either limiting the amount of food the stomach can hold, altering how food is digested, or both. Common types include gastric bypass, sleeve gastrectomy and adjustable gastric banding.
What are the risks and benefits of Bariatric Surgery?
The benefits of bariatric surgery include significant weight loss, improvement or resolution of obesity-related conditions, and enhanced quality of life. However, like any surgery, it carries risks, including infection, blood clots, nutritional deficiencies and complications from the procedure itself. It’s important to discuss all risks and benefits with a healthcare provider before deciding to undergo surgery.
How much weight can I expect to lose after Bariatric Surgery?
Weight loss varies by individual, but many people can expect to lose 50-70% of their excess weight within the first 12-18 months following surgery. Factors such as the type of surgery, adherence to diet and exercise plans and individual metabolism can all influence weight loss. It’s important to set realistic goals and understand that weight loss is gradual and requires ongoing effort.









