The Brandy lift was once marketed as a major advance in baldness treatment—a bold surgical option that, at the time, seemed to offer a definitive solution.
But years on, the long-term reality has come into sharper focus. Many patients who underwent this procedure decades ago are now dealing with side effects that weren’t fully understood—or disclosed—at the time.
In clinical practice today, we’re often asked to manage these legacy outcomes. The good news is that surgical repair and non-invasive therapies have come a long way. Even in cases where the scalp has been significantly altered by earlier interventions like the Brandy lift, it’s now possible to improve both the cosmetic appearance and underlying tissue health using modern techniques.
This guide provides a detailed overview of the original technique, the long-term complications many patients continue to face, and the advanced corrective options now available to restore a more natural and comfortable scalp.
What Is a Brandy Lift?
The Brandy lift—named after its creator, Dr. Dominic Brandy—was a widely performed scalp reduction technique during the 1980s and early ’90s, aimed at treating male pattern baldness. The procedure was ambitious in scope.
Surgeons would remove a large section of bald scalp, usually from the crown, then stretch and reposition the surrounding hair-bearing tissue from the sides and back to close the gap.
At the time, it was seen as an innovative way to restore coverage without relying on grafting. But the mechanical tension it placed on the scalp—and the long-term consequences—were not yet fully appreciated.
In 1993, Dr. Brandy published a series describing more than 1,200 cases. He highlighted the procedure’s ability to produce rapid coverage and significantly reduce the visible signs of baldness.
At the time, these outcomes were seen as a compelling alternative to the slower, more incremental results associated with traditional grafting techniques.
Why Problems Appear Years Later
In the early years, many patients felt satisfied with the results of a Brandy lift. But the issues don’t always show up right away. It’s often not until five, ten, or even twenty years later that the underlying problems begin to reveal themselves.
One of the most visible long-term consequences is the so-called slot scar—a linear indentation or seam that forms either at graft entry points or where opposing flaps of scalp were surgically joined.
Early on, surrounding hair can help disguise it. But as thinning progresses over time, especially in the zones adjacent to the scar, it becomes harder to conceal. What was once a hidden surgical line often becomes a prominent cosmetic concern.
Closures that were once tight and nearly invisible don’t always stay that way. Over time, as the scalp stretches and the surrounding tissue loses elasticity, these scars can widen. What begins as a faint line may evolve into a broad, smooth, reflective strip that’s difficult to hide.
In some cases, the repositioning of hair-bearing flaps alters the original growth pattern, causing follicles to grow against the natural direction. This mismatch can result in noticeably disrupted or even reversed hair flow across the scalp.
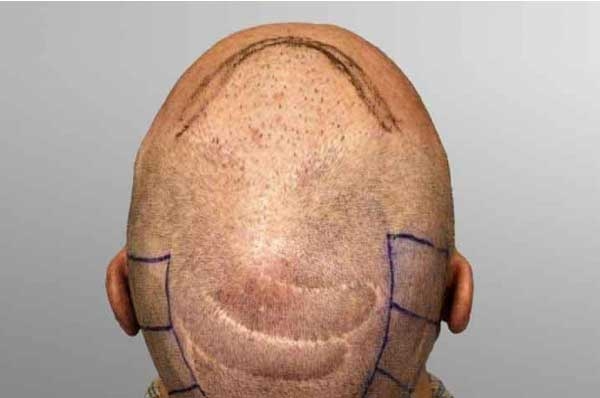
Assessing Your Scalp Today
Before moving forward with any form of corrective treatment, it’s crucial to first assess the present condition of the scalp. Both the patient and the clinician need a clear understanding of three core factors that will guide the repair strategy:
1. Vascularity
Healthy blood flow is fundamental to both healing and the survival of transplanted grafts. When circulation is compromised, new follicles may fail to anchor or thrive. This is especially relevant in scarred areas, where the microvascular network may be disrupted or partially collapsed—making successful graft uptake far less predictable.
To evaluate vascular health, clinicians often turn to imaging tools. Doppler ultrasound, for example, can map deeper blood flow patterns across the scalp, helping to identify regions that may require pre-treatment before any surgical repair is attempted.

2. Scalp Laxity
Scalp laxity refers to how freely the skin on the head can shift or stretch—something that becomes especially important when planning any kind of reconstructive work or hair transplant. It directly influences what techniques are viable and how much tissue can be safely mobilized.
A commonly used method for evaluating this is the Mayer-Pauls test. During the assessment, a clinician marks two fixed points on the scalp, compresses the tissue manually, and measures how much the distance between the marks shortens. The greater the reduction, the more flexible the scalp. And the more pliable the tissue, the more options a surgeon has—both in terms of access and technique.
3. Trichoscopy and Tissue Health
To properly assess the health of the scalp and follicles, we often rely on trichoscopy. It gives us a magnified view of the skin and hair units, helping us see whether follicles are still intact, have miniaturized over time, are missing altogether, or might still support future growth.
This level of detail is essential—it helps us decide if grafting is even worth considering or if a non-surgical route makes more sense.
Raposio and his team (2022) stressed how critical this kind of evaluation is, especially when planning complex procedures like scar revision or tissue expansion. And while severe scarring can look discouraging at first glance, it’s not always the end of the road.
With a measured, personalized approach, there’s often more potential for improvement than most patients expect.
Modern Repair Options
FUE into Scar Tissue
Follicular Unit Extraction (FUE) now plays a key role in addressing scalp scarring. Thanks to improvements in tools and techniques, surgeons can harvest individual follicular units from healthy donor areas and implant them directly into scarred or fibrotic zones with remarkable accuracy.
When blood supply in the recipient area is sufficient, these grafts tend to do well—survival rates in scar tissue typically fall between 80 and 90 percent.

Consistent outcomes depend on careful surgical planning. Every detail matters—from selecting the right punch size to fine-tuning the angle and depth of graft insertion.
Knowing when to hold back is just as important. Overpacking a scarred area can restrict blood flow and reduce graft survival, so density has to be managed thoughtfully.
This kind of strategic restraint becomes even more critical when donor hair is limited, which is often the case in patients who’ve previously undergone scalp-lifting procedures like the Brandy lift.
Laser-Assisted FUE
Using fractional CO₂ laser resurfacing to precondition scarred scalp tissue has shown real promise as a way to improve graft survival in FUE-based scar repair.
A 2024 randomized controlled trial by Xue and colleagues found a clear benefit: patients who received laser treatment before transplantation saw graft survival rates of 91%, compared to just 78% in those treated with FUE alone. The findings suggest that targeted laser therapy can enhance tissue receptivity and help set the stage for better outcomes.
The key to the laser’s effectiveness lies in how it works beneath the surface. By creating controlled microthermal injuries, the laser triggers localized neovascularization and softens dense fibrosis.
This remodeling process makes the area more biologically receptive, giving transplanted follicles a better chance to anchor, integrate, and grow successfully.
Fractional CO₂ Resurfacing
Fractional CO₂ laser treatment can also be used on its own to improve the appearance and structure of raised or fibrotic scars. While it doesn’t promote hair regrowth directly, its value lies in how it reshapes the scar tissue.
The therapy helps soften rigid texture, reduce surface elevation, and even out pigment irregularities. In doing so, it can transform areas that were once poor candidates for transplantation into sites that are far more suitable for grafting in the future.
SMP Camouflage
Scalp micropigmentation (SMP) is a technique that uses carefully placed pigment within the dermis to mimic the look of natural hair follicles. When done well, it can create the visual effect of increased density in thinning or scarred areas.
SMP tends to work especially well on pale or indented scars, and it’s often a good option for patients with lighter skin tones. It’s commonly applied to areas where traditional grafting may not be viable, such as the midline slot scar or the elevated nape, due to limited blood supply or compromised tissue quality.
Tissue Expansion and Grafting
For patients dealing with significant scarring and limited donor supply, tissue expansion can offer a practical surgical alternative. The process begins by placing expandable devices beneath sections of healthy, hair-bearing scalp.
These expanders are gradually inflated over time, encouraging the surrounding skin to stretch and generate new tissue, complete with viable follicles.
Once enough expansion has occurred, this newly formed scalp can be repositioned, either advanced or rotated, to cover areas affected by scarring or hair loss.
Combination Repair Plans
Many patients benefit most from a multi-step strategy. A typical sequence might involve:
- Fractional CO₂ resurfacing to soften scar tissue
- One or two FUE sessions to restore density
- SMP to blend residual contrast
The most effective treatment plan will depend on a combination of factors—your scalp’s condition, the availability of donor hair, and your individual goals.
A skilled surgeon will take all of this into account, shaping a strategy that aligns with your anatomy, medical history, and long-term expectations.
Real-World Case Study
A 52-year-old male presented with a history of Brandy lift surgery performed in 1991, accompanied by the following concerns:
- Prominent midline slot scar and unnaturally low hairline, measuring approximately 2–3 inches from the brow.
- CIT FUE technique was selected for graft extraction, ideal for scarred or tight donor zones. Over 1,600 follicular units were harvested without the need for strip excision.
- Hairline revision involved surgically elevating the frontal border and excising large, plug-like grafts. These were then redistributed further back to create a more age-appropriate frame.
- Two transplant sessions were performed. The updated hairline showed improved angulation, softer density gradients, and a more natural appearance overall.
- Camouflage strategy included placing single and double grafts around the larger units to blend them visually and soften the frontal edge.
- Post-operative recommendation included optional future refinement, such as selective graft softening or additional thickening. However, the patient was already satisfied with the cosmetic improvement.
Temple scars were left untreated at the patient’s request. These remained faint and well-disguised when the hair was worn long.




Cost, Downtime & Expected Results
| Procedure | Grafts / Sessions | Downtime | Cost Range (USD) |
| FUE into Scar Tissue | 1,000–2,000 | 7–10 days | $4,000-$15,000 |
| Laser-Assisted FUE | 1,500–2,000 | 7–10 days | $6,500–$10,000 |
| CO₂ Resurfacing | 3-5 sessions | 3–5 days | $3,000–$7,000 |
| SMP | 3-4 sessions | 1 day | $1,800-$4,000 |
| Tissue Expansion & Graft | 2 procedures | 6–8 weeks total | $4,000–$12,000+ |
Can scalp scars be completely removed?
Not entirely. While complete removal isn’t possible, most scars can be significantly improved.
With the right combination of treatments, many become softer, flatter, and well-blended—often to the point where they’re barely visible.
How many treatment sessions will I need?
It depends on the severity and type of scar, but most patients can expect at least 2 to 3 sessions spaced over 6 to 12 months.
The best results usually come from a multi-step approach that blends surgical techniques with non-surgical therapies.
Is a second scalp lift ever recommended?
Almost never. Repeating a scalp lift increases tension on the tissue and risks further reducing elasticity, which often makes the original issue worse, not better.
Is scalp micropigmentation (SMP) a permanent solution?
SMP is semi-permanent. While the results can last several years, most people will need maintenance or touch-ups every 3 to 5 years to keep the pigmentation looking natural and consistent.
How long is the recovery period?
Recovery varies depending on the procedure. After hair grafting, most patients are back to normal routines within 7 to 10 days. Laser treatments typically involve a shorter downtime—usually 2 to 3 days for most individuals.
Ready for a Second Chance?
You didn’t choose the complications you’re dealing with, but you do have control over what comes next.
With the advancements available today, there are effective ways to correct the outcomes of earlier procedures. Both surgical and non-surgical options can make a real difference.
Schedule a free consultation, and we’ll start by evaluating the current condition of your scalp. From there, we’ll create a tailored treatment plan—using the most refined techniques modern hair restoration has to offer.
References:
- BRANDY, DOMINIC A. “Scalp Lifting.” The Journal of Dermatologic Surgery and Oncology, vol. 19, no. 11, 1 Nov. 1993, pp. 1005–1014, https://doi.org/10.1111/j.1524-4725.1993.tb00992.x. Accessed 30 May 2025.
- Xue P, Yang Q, Guo L, Yin Y, Dou W, Li T, Zeng X, Song B, Fan X. Follicular unit extraction combined with fractional carbon dioxide laser therapy for post-traumatic eyebrow scar with defects: A prospective and comparative study. J Cosmet Dermatol. 2024 Dec;23(12):4146-4152. doi: 10.1111/jocd.16518. Epub 2024 Aug 11. PMID: 39129177; PMCID: PMC11626299.
- Chen L, Xu H, Wang QY, Chen P, Wang LQ, Qin XM. Treatment of Surgical Scars with Fractional Carbon Dioxide (CO2) Laser: A Randomized Controlled Trial. Adv Wound Care (New Rochelle). 2025 Jan 27. doi: 10.1089/wound.2024.0213. Epub ahead of print. PMID: 39869009.
- Raposio E, Raposio G. Scalp reconstruction by tissue expansion: tips and tricks. Acta Biomed. 2022 Oct 26;93(5):e2022313. doi: 10.23750/abm.v93i5.13393. PMID: 36300222; PMCID: PMC9686169.